Gut inflammation is a significant health concern linked to a spectrum of conditions, from acute discomfort to chronic disorders like Crohn's disease and ulcerative colitis. Our digestive health, immune responses, and systemic inflammation are influenced by the gut microbiome. Addressing gut inflammation supports wellness and reduces health issue impacts. So, what exactly do we mean by gut inflammation?
What is gut inflammation?

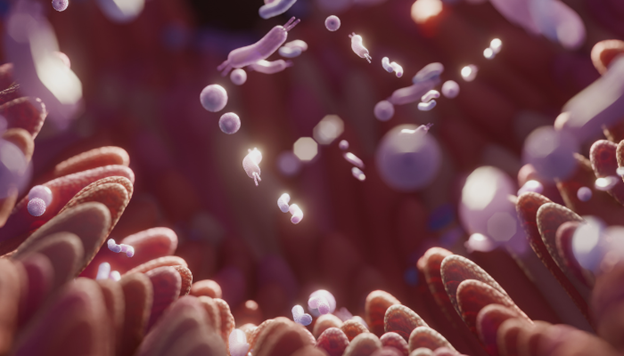
Gut inflammation refers to the body's immune reaction within the gastrointestinal (GI) tract, a vital system that begins at the mouth and extends to the anus, encompassing organs like the stomach and intestines.
This inflammation often arises from various triggers such as infections, autoimmune disorders, or exposure to irritants, leading to increased immune activity and tissue damage in the digestive tract. Common conditions associated with gut inflammation include Crohn's disease, ulcerative colitis and celiac disease.
The inflammatory response involves a surge in blood flow, immune cell activity, and cellular metabolism, working together to remove harmful stimuli and start the healing process.
Maintaining overall digestive health and preventing long-term complications requires effective management of gut inflammation.
How inflammation affects the gastrointestinal (GI) system
Gut barrier function: The intestinal lining serves as a critical barrier, blocking harmful substances from entering the bloodstream. Factors like an unhealthy diet or stress can compromise this barrier, leading to "leaky gut syndrome," where toxins and microbes leak into the bloodstream, inciting widespread inflammation.
Microbial balance: A balanced gut microbiota is essential for optimal immune function inflammation. Thus, fostering a healthy microbial environment is key to controlling inflammatory responses. Restore balance with The Good Bug's Gut Balance, designed to balance your gut microbiome effectively. It protects from digestive issues, boosts gut health, helps enhance metabolism, and promotes nutrient absorption
Production of Short-chain Fatty Acids (SCFAs): Beneficial gut bacteria ferment dietary fibers to produce SCFAs, such as butyrate, which possess potent anti-inflammatory effects and are vital for reinforcing the integrity of the gut barrier, thus preventing inflammatory triggers from escaping into the body.
Immune system modulation: The gut hosts a substantial part of the immune system, with the microbiome playing a crucial role in shaping immune responses. A well-regulated gut microbiota helps fine-tune immune reactions, ensuring that inflammation remains a targeted, rather than a generalized, response.
Inflammation damages the gut lining and alters normal gut flora. Chronic inflammation can lead to changes in the structure and function of the gut, including fibrosis (scarring) and the formation of ulcers. Let's look into the causes behind this inflammation.
Causes of gut inflammation
- Internal and external factors influencing gut bacteria balance
Diet, lifestyle, medication use, and exposure to pathogens play significant roles in maintaining the balance of gut bacteria. Disruptions can promote the growth of harmful bacteria, leading to inflammation. Poor diet and certain environmental exposures might trigger inflammation. A balanced diet complemented by targeted probiotics and prebiotics such as those from The Good Bug, can help mitigate these risks.
- Infections that damage the intestinal barrier
Infections from bacteria, viruses, and parasites can compromise the intestinal barrier, increasing gut permeability. This allows toxins and pathogens to enter the bloodstream, exacerbating inflammation.
- Impact of inflammatory bowel disease, like crohn’s disease and ulcerative colitis
Inflammatory bowel diseases (IBD) like Crohn's disease and ulcerative colitis involve chronic inflammation of the GI tract. These conditions are believed to stem from an abnormal immune response to intestinal microbiota in genetically predisposed individuals, leading to persistent inflammation that can severely affect the digestive system.
- Effects of certain medications on gut bacteria
Certain medications can disrupt the gut microbiome by killing beneficial bacteria. Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) may irritate the stomach lining and contribute to inflammation when used frequently. Discuss medication side effects with a healthcare provider.
- Damage from Refined Foods and Stress on the Intestinal Barrier
Refined sugars and fats promote harmful bacteria and inflammation. Similarly, chronic stress impacts gut health by weakening the immune response and enhancing gut permeability, further contributing to issues such as leaky gut and systemic inflammation.
Inflammatory diseases affecting gut
- Celiac disease: Triggered by gluten, this autoimmune disorder damages the small intestine, leading to diarrhea, bloating, and nutrient absorption issues. It is diagnosed through antibody tests and intestinal biopsies and managed with a strict gluten-free diet.
- Gastroenteritis: Often resulting from infections, this condition inflames the stomach and intestines, causing symptoms like diarrhea, vomiting, and dehydration. It is diagnosed based on medical history and physical exams, with treatment focused on rehydration and, if necessary, medications.
- Ulcerative colitis: A form of IBD affecting the colon and rectum, this disease causes ulcers and inflammation that lead to bloody diarrhea and abdominal pain. It is diagnosed with lab tests and imaging, with treatments ranging from medications to surgery for severe cases.
- Diverticulitis: Involving inflammation or infection of the diverticula in the colon, this condition manifests as lower abdominal pain and fever. Diagnosed through physical exams and imaging, it is treated with antibiotics, dietary adjustments, and sometimes surgery in severe cases.
Internal and external factors influencing gut bacteria balance
Factors such as diet, lifestyle, medication use, and exposure to pathogens significantly influence the balance of gut bacteria. Disruptions in this balance can lead to an overgrowth of harmful bacteria, which triggers inflammation.
Factors affecting gut bacteria balance
Antibiotic use
Antibiotics are vital for treating infections but they also disturb the gut microbiota by killing both harmful and beneficial bacteria. This disruption can cause a temporary decline in beneficial bacteria such as Bifidobacteria and Lactobacilli and may lead to long-term changes in the gut flora. Managing the effects can help maintain a healthier gut microbiome and prevent further complications.
Lack of prebiotics in the diet
Prebiotics are dietary fibers found in foods like lentils, oats, and bananas that support beneficial gut bacteria. A diet lacking in prebiotics can disrupt digestive health, affecting the balance and functionality of the gut microbiome. For busy individuals seeking convenient fiber sources, consider prebiotic-rich snack bars. The Cocoa and nut prebiotic bars & Mixed Berry & Nuts Prebiotic Bars from the Good Bug provides 1/3rd portion of daily fiber needs while potentially supporting gut health.
Food additives
Certain food additives, including emulsifiers and artificial sweeteners, can negatively impact the gut microbiota, leading to inflammation and other digestive issues. Limiting these additives may be beneficial for gut health.
Cooking and processing methods
Cooking methods can differentially affect the gut microbiome. Techniques like roasting can increase the abundance of beneficial bacteria, whereas boiling might not have the same effect, showing the importance of cooking methods on gut health.
Exercise

Regular exercise promotes a balanced and diverse gut microbiota. However, the intensity of physical activity should be considered to avoid potential adverse effects on gut health. Enhance your exercise routine with The Good Bug's Metabolic Fiber Boost designed to balance your gut microbiome, boost metabolism, and reduce food cravings.
Stress
Stress directly impacts the gut microbiome, affecting overall health. Managing stress is crucial for maintaining a healthy gut, which can also help improve emotional resilience.
Recovery from antibiotics
After antibiotic use, integrating probiotics and increasing dietary fiber can help restore and maintain a healthy gut microbiome. Avoiding unnecessary antibiotics can also prevent imbalances in gut flora.
Symptoms of gut inflammation
Symptoms of gut inflammation can vary widely among individuals, depending on the cause, location, and severity of the inflammation.
- Abdominal pain: Discomfort or cramping in the stomach area.
- Bloody stools: Presence of blood in the stool, which may indicate damage to the intestinal lining.
- Persistent diarrhea: Frequent loose stools that continue over a period of time.
- Weight loss: Unintended loss of weight which may stem from malabsorption of nutrients due to gut inflammation.
- Fatigue: General tiredness and a lack of energy, often resulting from the body's response to inflammation.
- Fluctuating symptom intensity: Symptoms may vary in severity and can worsen during periods known as flare-ups.
- Severe symptoms: Frequent bloody stools or significant weight loss can be signs of more extensive damage and should be addressed promptly.
Diagnosis of inflammatory bowel disease
Diagnosing inflammatory bowel disease (IBD) involves a combination of medical history review, physical examinations, and diagnostic tests to understand the symptoms' onset, type, and progression. Here's a structured approach to how IBD is typically diagnosed:
Medical history and symptom review: This initial step assesses the type and progression of symptoms to guide further diagnostic testing.
Blood and stool tests:
- Blood tests help detect inflammation through markers like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), and a complete blood count can indicate inflammation presence and assess overall health.
- Stool samples are analyzed for hidden blood and to exclude infections caused by bacteria, viruses, or parasites.
Endoscopic examinations:
- Doctors use colonoscopy to directly visualize the colon and collect biopsy samples to confirm inflammation and distinguish it from other conditions. An upper GI endoscopy may be performed to examine the stomach and small intestines, sometimes using a camera capsule swallowed by the patient.
Imaging tests:
- Detailed imaging like barium X-rays provide comprehensive views of the gastrointestinal tract, complemented by advanced techniques such as ultrasound, CT scans, and MRIs to identify complications and assess the extent of inflammation.
These diagnostic tools and procedures help in accurately diagnosing IBD, facilitating effective management and treatment planning to alleviate symptoms and prevent serious complications.
Dietary changes to manage gut inflammation
Adopting a nutrient-dense, anti-inflammatory diet
- To manage gut inflammation effectively, adopting a diet rich in nutrients that support gut health is essential. To manage gut inflammation effectively, adopting a diet rich in nutrients that support gut health is essential. This includes consuming foods that help repair the gut lining and reduce inflammation.
Incorporating key anti-inflammatory foods
- Focus on integrating foods with anti-inflammatory properties into your diet. This includes turmeric, ginger, omega-3 fatty acids from fish like salmon and sardines, and flaxseeds, which all contribute to reducing gut inflammation and supporting overall gut health.
Reducing intake of foods that exacerbate inflammation
- Limit your consumption of ultra-processed foods and those high in refined sugars and saturated fats, such as white bread, pastries, processed meats, and fast foods. These can worsen gut inflammation and disrupt the balance of gut bacteria.
Benefits of balanced meals and frequent eating
- Patients with gut inflammation often find that smaller, more frequent meals are more comfortable to digest. This eating pattern not only reduces the strain on the digestive system but also ensures a steady intake of nutrients throughout the day to combat inflammation.
Moderation in consumption of challenging foods
- While completely eliminating favorite foods isn't necessary, moderating the intake of potentially problematic foods like spicy dishes or red meat can help manage symptoms of gut inflammation without giving up cultural or preferred foods entirely. Opt for adapting recipes or reducing portion sizes to lessen their impact.
Enhancing diet with omega-3 and fermented foods
- Including more omega-3 fatty acids can significantly affect reducing gut inflammation. Foods rich in these healthy fats, such as mackerel, herring, and other oily fish, are beneficial. Additionally, incorporating fermented foods like yogurt and kefir improves gut health further aiding in inflammation reduction.
Consider nutritional supplements
- If appetite is low and consuming solid foods is challenging, consider incorporating nutritional supplements or liquid meal replacements. These can provide essential nutrients without causing additional strain on the digestive system.
Through these dietary adjustments, managing gut inflammation becomes more feasible, contributing to overall health and reducing the risk of chronic inflammation-related complications.
Probiotics and their role in gut health
Probiotics are beneficial bacteria that, when ingested through supplements or certain foods, help restore and maintain the balance of gut microbiota, thus enhancing digestion and gut health. Prebiotics, on the other hand, are types of dietary fibers that feed these beneficial bacteria. Boost your gut health with the Daily Probiotics from The Good bug tailored to keep your gut flora thriving.
Benefits of probiotics in the diet
Introducing probiotics into your diet can significantly improve gut health by rebalancing gut flora. This restoration is key in mitigating gut inflammation and enhancing the function of the intestinal barrier, which protects against harmful substances entering the bloodstream.
Supporting beneficial gut bacteria growth
Probiotics actively promote the growth of beneficial gut bacteria, essential for maintaining the integrity of the gut and optimal immune function. This support is vital for controlling gut inflammation and ensuring a healthy digestive system.
Immune modulation and inflammation regulation
Probiotics play a pivotal role in modulating the immune system. They help decrease the production of inflammatory cytokines, which are responsible for gut inflammation, while increasing the production of anti-inflammatory cytokines that help soothe the gut. Support your body's natural defenses and promote immune health with The First Defense from The Good Bug.
Strengthening the intestinal barrier
Probiotics enhance the gut lining integrity, creating a robust barrier that prevents harmful pathogens and toxins from entering the bloodstream, which reduces the risk and severity of gut inflammation.
Incorporating probiotics into your diet not only helps in managing gut inflammation but also supports overall digestive health and immune function.
Lifestyle modifications for managing gut inflammation
Identifying and eliminating trigger foods
- To effectively manage gut inflammation, it’s crucial to identify and eliminate foods that exacerbate symptoms. Temporarily removing potential irritants like dairy or gluten can help pinpoint triggers and adjust your diet accordingly.
Prioritizing hydration
- Staying hydrated is essential for digestive health and helps maintain the mucosal lining of the intestines, which is vital in reducing gut inflammation
Mindful eating and physical activity
- Eating slowly and chewing thoroughly aids digestion and nutrient absorption, which can improve gut health. Coupling this practice with regular physical activity enhances overall health and helps manage symptoms of inflammatory bowel disease (IBD).
By implementing these lifestyle modifications, individuals can significantly impact their management of gut inflammation, enhancing their quality of life and overall health.
Practice Stress-Reducing Activities: Meditation, Yoga, Deep Breathing
Regular exercise for gut health
Engaging in regular physical activity like brisk walking, jogging, or cycling for at least 150 minutes per week is known to foster a healthier gut microbiota. Exercise not only enhances digestion but also helps reduce gut inflammation and improves overall gut health.
Stress management techniques
Chronic stress adversely impacts gut health, exacerbating gut inflammation. Practicing stress-reduction techniques such as meditation, deep breathing exercises, and yoga can significantly lower stress levels and promote a healthier gut. Incorporating hobbies and activities that you enjoy can also play a crucial role in managing stress and reducing its effects on gut inflammation.
Yoga’s dual benefit
Yoga serves as a powerful tool for stress reduction and physical health. It combines physical postures, breathing exercises, and meditation to improve overall well-being. Regular yoga practice can help strengthen the digestive system and alleviate symptoms of gut inflammation by enhancing blood flow and reducing stress.
Prioritizing adequate sleep
Quality sleep supports gut health and prevents inflammation. Disrupted sleep patterns can lead to an imbalance in gut microbiota and increase the risk of gut inflammation. Aim to get 7-8 hours of uninterrupted sleep each night to help your digestive system recover and reduce inflammation.
By adopting these lifestyle changes, you can effectively manage symptoms of gut inflammation and contribute positively to your overall digestive health. That's how lifestyle changes play a role, but what about the mental side of things?
Understanding the link between stress and increased risk of gut inflammation.
Chronic Stress and Inflammation
Persistent stress leads to chronic activation of this response, setting off prolonged inflammatory reactions. Inflammation is the body’s instinctive reaction to perceived threats, which can include physical invaders like viruses or emotional stressors.
The immune system releases pro-inflammatory cytokines to combat these threats. However, chronic inflammation can lead to a leaky gut, where the intestinal barrier becomes compromised, impairing nutrient absorption and increasing susceptibility to mental health disorders.
Did you know?
When you experience butterflies in your stomach or go with your gut feeling, it's due to your gut's own brain. Embedded within your digestive system, this second brain profoundly influences your mood, health, digestion, and thought processes.
Gut-brain connection
The gut is often referred to as the "second brain" due to its ability to produce neurotransmitters similar to those found in the brain, including serotonin, dopamine, and gamma-aminobutyric acid. These neurotransmitters are crucial for mood regulation. About 90% of the body's serotonin is synthesized in the digestive tract.
The connection between the gut and the brain is significant, mediated by pathways like the vagus nerve, which directly links the two organs. The gut microbiome plays a crucial role in this relationship by influencing brain function and emotional stability through mechanisms such as the production of short-chain fatty acids (SCFAs).
Prevention and early diagnosis
Effectively managing gut inflammation requires early diagnosis and prompt intervention. It is crucial to contact a healthcare provider early when symptoms such as severe abdominal pain, blood in the stool, significant weight loss, or unexplained changes in bowel habits worsen.
These symptoms could indicate serious conditions such as infections, inflammatory bowel disease (IBD), or even cancer, and require immediate medical examination. Seeking medical evaluation promptly helps determine the underlying causes and allows for the appropriate treatment to prevent complications and improve health outcomes.
Treatment Options for Inflammatory Bowel Disease
The primary treatment goal for inflammatory bowel disease is to reduce inflammation that triggers symptoms. Treatment plans may include:
Doctors treat inflammatory bowel disease (IBD) with medications, dietary adjustments, and sometimes surgery to alleviate symptoms, prevent complications, and potentially heal the intestines. Doctors might recommend the following treatments:
- Anti-inflammatory drugs to reduce inflammation
- Immunosuppressants to inhibit the immune system from triggering inflammation
- Biologic agents to target and block inflammation-causing proteins
- Nutritional therapy to allow the intestines to recuperate
Challenges like poor appetite, diarrhea, and ineffective nutrient absorption can make it difficult for individuals with IBD to obtain adequate calories and nutrients.
- Anti-inflammatory medications to manage inflammation.
- Immune system suppressants that help control the immune response preventing frequent flare-ups.
- Depending on the individual's symptoms, additional treatments may include antibiotics, anti-diarrheal medications, laxatives, pain relievers, and vitamin supplements.
In more severe cases, hospitalization may be required to administer treatments such as intravenous fluids or to perform surgery. Treatment typically involves a multidisciplinary team approach, including the expertise of a gastroenterologist and possibly a surgeon, alongside your primary care provider.
Managing Crohn's disease and other forms of inflammatory bowel disease requires a comprehensive and personalized approach to effectively control symptoms and maintain quality of life.
Managing gut inflammation effectively involves a combination of dietary adjustments, lifestyle changes, and, when necessary, medical interventions. Adopting an anti-inflammatory diet, incorporating probiotics, and managing stress are key strategies for reducing gut inflammation and promoting long-term health.
Emphasizing early diagnosis, appropriate dietary changes, and proactive lifestyle adjustments can significantly mitigate the impact of this condition. Integrating strategies such as maintaining a balanced diet, engaging in regular physical activity, and adopting stress-reduction techniques plays a pivotal role in controlling inflammation and enhancing life quality. For those looking to support their gut health further, exploring The Good Bugs range of products might provide additional benefits in managing gut inflammation effectively.
References:
https://www.centenary.org.au/health-hub/inflammation/good-gut-anti-inflammatory-diet/
https://www.medicalnewstoday.com/articles/gut-microbiome-may-influence-stress