Gut health is a cornerstone of your overall well-being. It plays a vital role in digestion, immune system function, mental health, and even hormonal balance. Your gut contains trillions of microorganisms, collectively known as the gut microbiota, which work together to maintain the balance of your body. But with rising issues like digestive disorders, antibiotic overuse, and stress, maintaining this balance can be tricky.
That’s where understanding the difference between antibiotics and probiotics becomes critical. These two agents interact with your gut microbiota in vastly different ways, and knowing how to use them correctly can make a significant difference in your health journey.
Key takeaways
-
Antibiotics are used to eliminate harmful bacteria during infections, but they can also disrupt the gut microbiota, causing side effects such as diarrhea and lowered immunity
-
Probiotics are live beneficial microbes that help restore gut balance, support digestion, and improve immunity, especially helpful after antibiotic use
-
The key difference is that antibiotics fight bacteria, while probiotics feed and support beneficial bacteria to maintain gut health
-
You can take probiotics alongside antibiotics, but it's best to do so with proper timing, ideally 2–3 hours apart, to ensure effectiveness
-
Support your gut naturally with fermented foods and science-backed probiotic supplements, such as those from The Good Bug, for long-term gut and overall well-being
What are antibiotics?
Antibiotics are medications used to treat bacterial infections. They work by either killing bacteria or inhibiting their growth. Developed in the early 20th century, antibiotics revolutionized medicine, saving millions of lives from once-fatal diseases.
Types of antibiotics
Antibiotics can be grouped based on their mechanism of action and range of bacterial targets:
-
Broad-spectrum antibiotics: Effective against a wide variety of bacteria, including both Gram-positive and Gram-negative strains
Example: Amoxicillin. These are commonly used when the specific bacteria causing the infection are unknown.
-
Narrow-spectrum antibiotics: Target specific types of bacteria, making them more precise and less disruptive to beneficial bacteria
Example: Penicillin G. They’re ideal when the exact bacteria are identified through testing.
-
Bactericidal antibiotics: Kill bacteria outright by attacking their cell walls or critical functions, such as DNA replication
-
Bacteriostatic antibiotics: Inhibit the growth or reproduction of bacteria, allowing the immune system to eliminate the remaining infection
Despite their effectiveness, antibiotics should be used carefully to minimize side effects, prevent the development of resistance, and maintain a balance in gut flora.
Also Read: Factors that Influence the Gut Microbiota
What are probiotics?
Probiotics are live microorganisms, often referred to as “good” or “friendly” bacteria, that provide health benefits when consumed in adequate amounts. Unlike antibiotics, which destroy bacteria, probiotics introduce or replenish beneficial microbes in your digestive system.
Common types of probiotic strains
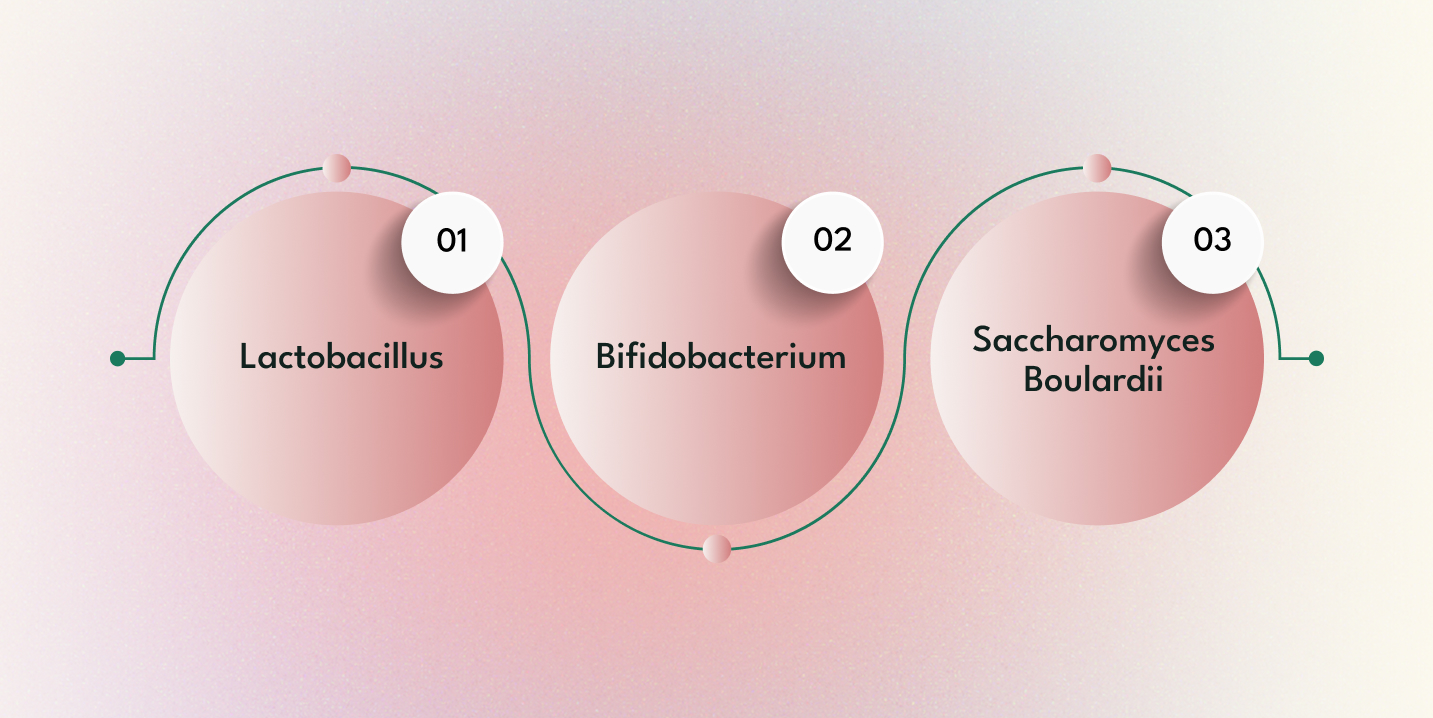
Each probiotic strain offers unique health benefits. Here are a few of the most widely studied and used:
-
Lactobacillus: Commonly found in yogurt and other fermented foods, this strain aids digestion, particularly in breaking down lactose. It can also help reduce diarrhea and support a healthy gut lining
-
Bifidobacterium: Naturally present in the intestines, this strain helps fight off harmful bacteria, supports the immune system, and is often used to manage symptoms of IBS (Irritable Bowel Syndrome)
-
Saccharomyces boulardii: A beneficial yeast, not a bacterium, known for its ability to treat and prevent diarrhea, especially antibiotic-associated and traveler’s diarrhea. It also helps protect the intestinal barrier
Together, these strains contribute to improved digestion, enhanced immunity, and a balanced gut microbiome, making probiotics a vital component in maintaining digestive health.
Also Read: The Gut Through Life Stages
What is the difference between antibiotics and probiotics?
Simply put, antibiotics fight bacteria, while probiotics feed bacteria.
|
Feature |
Antibiotics |
Probiotics |
|
Purpose |
Designed to eliminate harmful bacteria causing infections. They are used as a treatment to battle acute bacterial illnesses |
Intended to support and nurture beneficial gut bacteria. They help maintain or restore balance in your microbiota, promoting long-term digestive and immune health |
|
Mechanism |
Work by killing bacteria directly (bactericidal) or by inhibiting their growth (bacteriostatic). Their action is non-selective and may impact both harmful and beneficial bacteria |
Work by introducing beneficial bacteria into the gut, helping to rebuild the natural microbial balance that may have been disrupted by illness, stress, or antibiotic use |
|
Effect on Gut |
While effective in treating infections, they can also disrupt the gut flora by reducing bacterial diversity, which may lead to side effects such as digestive upset |
They help restore and maintain a healthy balance in the gut, improving digestion, supporting the immune system, and reducing symptoms of gastrointestinal distress |
|
Use Case |
Primarily used to treat bacterial infections, such as strep throat, pneumonia, or urinary tract infections, where rapid elimination of bacteria is critical |
Used as a preventive measure to alleviate digestive issues, boost immunity, and restore gut health, especially after treatment with antibiotics or during times of stress |
|
Prescription |
Typically require a doctor’s prescription and should be taken exactly as directed to ensure effectiveness and prevent the development of resistance |
Widely available over-the-counter, either in naturally fermented foods (like yogurt or sauerkraut) or as dietary supplements, making them accessible for daily use |
So, what is the difference between antibiotics and probiotics? Essentially:
-
Antibiotics serve as a curative tool aimed at eliminating harmful bacteria quickly during an active infection. Their decisive action, however, can sometimes result in collateral damage to the beneficial bacteria in your gut
-
Probiotics form more of a preventive and restorative measure. They work by replenishing and supporting the beneficial bacteria that contribute to a balanced microbiome, ultimately helping your gut recover and function optimally
This side-by-side understanding highlights that while antibiotics are crucial for immediate treatment, probiotics play a vital role in maintaining long-term gut health and overall well-being.
Also Read: A Brief Introduction to the Gut-Organ Axis
How antibiotics affect your gut
While antibiotics are highly effective at eliminating harmful bacteria responsible for infections, they often act indiscriminately, affecting both dangerous and good bacteria in your gut.
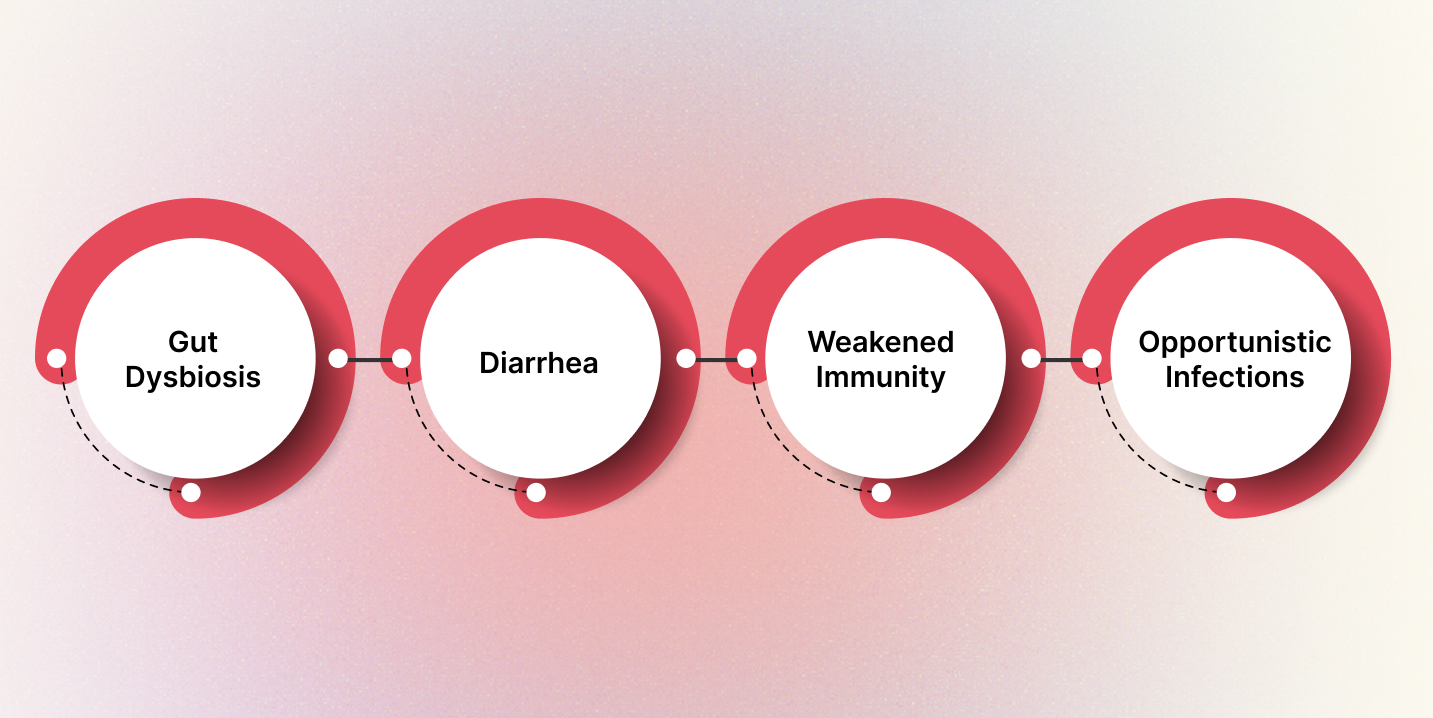
This lack of selectivity can lead to several side effects that disrupt gut health:
-
Gut dysbiosis: A condition where the natural balance of gut bacteria is disturbed. This imbalance can cause digestive discomfort, reduced nutrient absorption, and an increase in harmful bacteria
-
Diarrhea is one of the most common side effects of antibiotics. It occurs when beneficial bacteria are eliminated, allowing opportunistic bacteria to disrupt digestion and water balance
-
Weakened immunity: Since a significant portion of the immune system is located in the gut, a disruption in gut bacteria can impair the immune response, making the body more susceptible to further infections
-
Opportunistic infections: Pathogens like Clostridium difficile (C. diff) can take advantage of the reduced competition in the gut and overgrow, leading to severe inflammation and illness
These potential impacts underscore the importance of approaching the prolonged or frequent use of antibiotics with caution. Supporting your gut with probiotics during and after antibiotic use can help mitigate these effects and promote recovery.
How do probiotics benefit the gut?

Probiotics provide a gentle yet effective way to rebalance and reinforce your gut microbiome, particularly after antibiotics, illness, or stress have disrupted it.
-
Restoring microbial balance: After antibiotics or digestive issues, probiotics help repopulate your gut with beneficial bacteria, restoring the balance essential for healthy digestion and immunity
-
Improving digestion: They aid in breaking down complex food components, facilitating better nutrient absorption and reducing issues like bloating, constipation, and gas
-
Enhancing immunity: Probiotics interact with immune cells and help stimulate the production of protective antibodies, bolstering your body’s defense mechanisms
-
Preventing and treating diarrhea: Especially useful in managing antibiotic-associated diarrhea and traveler's diarrhea, probiotics help restore normal bowel function
-
Reducing inflammation: Regular use may help alleviate chronic gut inflammation associated with conditions such as IBS, Crohn’s disease, and ulcerative colitis, promoting long-term digestive comfort
Understanding the difference between antibiotics and probiotics is crucial. While antibiotics eliminate bacteria, probiotics restore and support the ecosystem, helping the gut function efficiently and recover from disruptions.
When to use antibiotics
Antibiotics are a vital tool in modern medicine, but they should be used with caution and only when necessary.
-
A confirmed bacterial infection is present, Such as strep throat, bacterial pneumonia, urinary tract infections, or skin infections, where bacterial involvement is apparent and verified by a healthcare provider
-
The benefits outweigh the risks of gut disruption: In severe infections, the immediate need to eliminate harmful bacteria takes priority, even if it means temporarily disrupting the gut microbiome
-
A healthcare professional prescribes them: Antibiotics must be taken only under medical supervision, after ruling out viral infections (e.g., colds, flu), which do not respond to antibiotics
Overuse or self-prescription can lead to antibiotic resistance, a growing global health threat where bacteria evolve to survive medication, making future infections more difficult to treat. This is why understanding their role and pairing them wisely with probiotics is essential for maintaining overall health.
Also Read: All About Probiotics
When to use probiotics
Consider incorporating probiotics into your routine during times when your gut balance is challenged.
-
You’re on or have just completed a course of antibiotics: Antibiotics can deplete your good gut bacteria. Probiotics help replenish this loss and reduce the risk of antibiotic-associated diarrhea or other digestive issues
-
If you suffer from chronic digestive issues, such as IBS, bloating, or constipation, probiotics can help regulate bowel movements, reduce bloating, and alleviate abdominal discomfort by restoring microbial balance
-
You have weakened immunity and want to improve gut health: Since much of the immune system resides in the gut, a healthier microbiome may enhance your body’s natural defenses against infections and inflammation
-
You consume a low-fiber or highly processed diet: These diets don’t support microbial diversity. Probiotics can help counteract poor nutrition by reintroducing beneficial strains into the gut
-
You want to support overall mental health and mood (gut-brain axis): An imbalanced gut has been linked to anxiety and depression. Probiotics may help regulate neurotransmitter activity through the gut-brain connection
This distinction highlights the difference between antibiotics and probiotics. While antibiotics are used in the short term to fight infections, probiotics offer long-term support for digestive, immune, and mental well-being.
Can you take probiotics and antibiotics together?
Yes, and often it’s recommended. Taking probiotics alongside antibiotics can help mitigate the adverse effects that antibiotics have on your gut.
-
Reduce the risk of diarrhea, especially antibiotic-associated diarrhea, which is common due to the disruption of gut bacteria
-
Help replenish beneficial bacteria: By reintroducing healthy microbes into the gut, probiotics restore balance lost during antibiotic treatment
-
Support faster gut recovery: They help repair the gut lining, restore digestion, and reduce inflammation, speeding up your return to normal health
However, timing is key. To avoid probiotics being neutralized by the antibiotic, take them at least 2–3 hours apart from your antibiotic dose. This spacing helps ensure the survival and effectiveness of the probiotic strains.
Food sources of probiotics
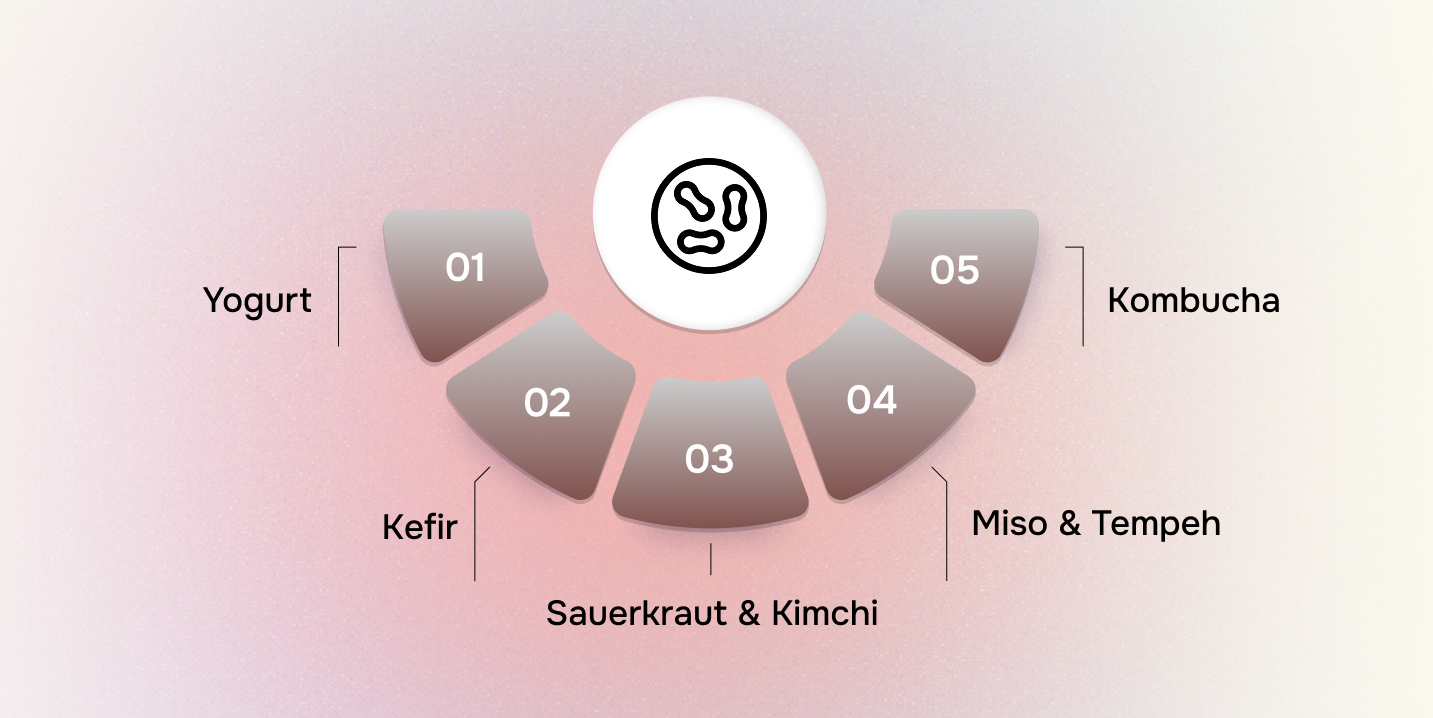
You don’t always need supplements to get your daily dose of good bacteria. Many fermented foods naturally contain probiotic strains and can be easily included in your diet:
-
Yogurt: A well-known source of probiotics, especially those with live and active cultures like Lactobacillus and Bifidobacteria. Choose unsweetened, plain versions for maximum benefit
-
Kefir: A tangy, drinkable yogurt made from fermented milk, often containing more strains and higher probiotic content than regular yogurt
-
Sauerkraut & kimchi: These fermented cabbage dishes are rich in lactic acid bacteria and offer a spicy or tangy boost to gut health
-
Miso & tempeh: Traditional fermented soy products packed with nutrients and beneficial bacteria. They also serve as excellent sources of plant-based protein
-
Kombucha: A fermented tea beverage known for its slightly fizzy texture and live cultures, supporting digestive and liver health
Incorporating these foods regularly helps maintain a balanced gut microbiome and is a natural, delicious way to support gut health, especially when recovering from antibiotic use.
Also Read: 20 Best Probiotic Foods and Easy Ways to Include in Your Diet
Choosing the right probiotic supplement
Not all probiotic supplements are equally effective, so it's essential to select one that meets your specific health needs.
-
Multiple strains: A variety of strains, such as Lactobacillus and Bifidobacterium, offer broader benefits by targeting different parts of the gut and supporting various functions, including digestion, immunity, and the control of inflammation
-
High CFU count: Look for supplements with at least 1 billion CFUs (colony-forming units) per serving. A higher count increases the likelihood that enough live bacteria reach your intestines to be effective
-
Enteric-coated capsules: These capsules are specially designed to withstand stomach acid, ensuring the bacteria reach the intestines where they’re needed most
-
Scientifically supported strains: Select products featuring clinically studied strains, such as Lactobacillus rhamnosus GG or Saccharomyces boulardii, which have been proven to offer benefits for gut recovery, immunity, and diarrhea prevention
If you're currently on antibiotics, it’s best to consult your doctor or pharmacist to determine which probiotic strains are most compatible and effective during and after treatment.
Whether you're recovering from antibiotic use, dealing with digestive issues, or simply looking to improve your gut wellness long-term, The Good Bug has you covered.
Their products are thoughtfully formulated with clinically researched probiotic strains, prebiotics, and essential nutrients to support various aspects of health, including digestion, immunity, energy levels, and mental well-being.
Explore The Good Bug’s range today and experience what true gut wellness feels like because a healthier gut means a healthier, happier you. Shop Now at The Good Bug!
FAQs
1. What is the main difference between antibiotics and probiotics?
Antibiotics kill or stop the growth of harmful bacteria during infections, whereas probiotics introduce or support beneficial bacteria to maintain a healthy gut.
2. Can I take probiotics and antibiotics at the same time?
Yes, but you should space them out by at least 2–3 hours. This prevents the antibiotic from killing the beneficial probiotic bacteria, supporting better gut recovery.
3. What are the common side effects of antibiotics on gut health?
They can cause gut dysbiosis, diarrhea, reduced immunity, and even opportunistic infections like C. difficile overgrowth due to a drop in beneficial bacteria.
4. Which foods are naturally rich in probiotics?
Yogurt, kefir, kimchi, sauerkraut, miso, tempeh, and kombucha are excellent fermented foods rich in live cultures that support gut health.
5. How do I choose a good probiotic supplement?
Look for multiple strains, high CFU count (1 billion+), enteric-coated capsules, and scientifically supported strains like Lactobacillus rhamnosus GG or Saccharomyces boulardii. For a trusted option, explore The Good Bug’s gut-focused range.


